Are you struggling to lose weight despite all the slim shakes, restrictive diet, and intense workouts you’ve tried? Sometimes it isn’t because of what you have or haven’t done. It is what’s going on in your body that thwarts your progress in weight management. Polycystic ovary syndrome, also known as PCOS is one of the conditions that would make losing weight more difficult than healthy individuals.
What is PCOS?
PCOS is a type of hormonal disorder that commonly occurs in women at their reproductive age. The exact cause of PCOS is unknown. Women with PCOS present with a high level of androgen and insulin resistance, meaning the body cannot use insulin built up in their bloodstream. These two abnormal levels make weight loss more difficult because they both lead to fat-storing in the body.
Therefore, women with PCOS also have a higher rate of weight gain, overweight, obesity, and central obesity compared to those without PCOS. Obesity and insulin resistance tends to further exacerbate the symptoms of PCOS and the risk for Type 2 diabetes and cardiovascular disease, and also increase metabolic syndrome including high blood pressure, or abnormal blood lipid levels.
Symptoms of PCOS
If you are suffering from the symptoms below, it’s likely that PCOS is taking place on you.
- Missed or irregular periods
- Large ovaries or ovaries carrying cysts
- Excess body hair
- Gain weight easily, especially around the belly
- Acne or oily skin
- Baldness or thinning hair
- Infertility
- Skin tags on neck or armpits
- Dark or thick skin patches on the neck, armpits or under the breast
It doesn’t mean that any of the symptoms above surely lead to PCOS while if you’re suffering from one or a few of the symptoms, it’s the right time to consult your doctor.
How does Intermittent Fasting Manage with PCOS?
PCOS can be managed by diabetes medication and lifestyle changes to assist weight loss, reduce symptoms, improve insulin sensitivity and glycemic control. In fact, a 5-10% weight loss can reduce symptoms of PCOS, improve metabolic marker and other complications and the essential benefit of intermittent fasting lies in its function in weight control. Moreover, intermittent fasting can be used to improve insulin resistance and reduce calories intake for weight loss in order to manage PCOS.
Intermittent fasting aims to extend fasting time and reduce food intake naturally by restricting the eating time. The energy restriction during fasting can reduce blood glucose levels and improve insulin sensitivity. A recent study has found that following 8-hour time restricted feeding for 5 weeks significantly reduced body weight, body fat, improve insulin resistance, androgen level, and chronic inflammation in women with PCOS.
Other Things to Combine with Intermittent Fasting to Manage PCOS
Apart from fasting, there are other lifestyle modifications you can combine with intermittent fasting to improve your metabolic profile to manage PCOS.
Less carbohydrate intake or low carbohydrate diet
The amount of carbohydrates you eat is directly linked to your insulin level and blood sugar management. A low-carb or carb-restricted diet involves reducing carbohydrate intakes such as high-carb foods like bread, rice, pasta, some starchy vegetables, sweets, and sugary drinks. This is often recommended to help blood sugar control, improve insulin sensitivity and promote weight loss for Type 2 Diabetes and manage PCOS.
A traditional low carbohydrate diet such as Keto, limits intake of carbohydrates to 20-50 grams daily, which is difficult to follow in the long term. Therefore, the diet should be upgraded.
Instead of starting on such intense carb restriction, you can start with 2 simple steps:
| Limit | Swap |
| Refined carbohydrate intake in your diet Sugar/added sugar Sugar-sweetened beverages Bakery and desserts Sugary cereals white/refined grains | Swap at least half a portion of your regular carbs, such as potato, pasta, rice, and bread to Non-starchy vegetables, such as zucchini, tomato, bell pepper, leafy greens, mushrooms, and cruciferous veggies (broccoli, cauliflowers) Legumes Fruits |
Low Glycemic Index
The type of carbohydrate also plays an important role. Glycemic index (GI) refers to a measure of how quickly a food causes your blood sugar level to rise. Foods with higher GI are more quickly digested and absorbed causing a rapid rise in blood sugar level. Low GI foods are rich in fiber, therefore more difficult to digest, and have a slower effect.
Choosing low GI food during your eating window can help you further manage insulin resistance by lowering insulin levels:
| Low GI | Medium GI | High GI |
| Most fruits & vegetables Legumes Whole grains & cereals Dairy Multigrain & seeds Wholemeal pasta | Wholemeal grains Some starchy vegetables Some fruits (rockmelon, apricots) Refined grains & cereals (couscous, gnocchi) Condensed milk | Sugar Sugar-sweetened beverages Sugary desserts Refined grains (white rice) Sugary cereals |
Other ways to lower the GI of your meal:
- Add vinegar or lemon juices as dressing
- Add more fiber
- choose “high fiber” whole-grain bread or cereals.
- Add fruits, vegetables, legumes, or psyllium husk fiber supplement.
- Add protein to your meal
- Cooked then cooled rice, potato or any other carbs
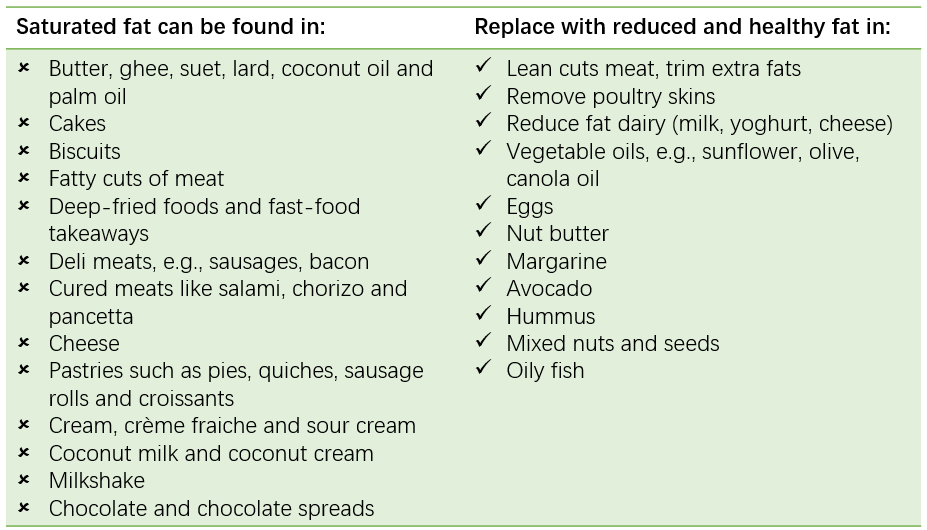
Low Saturated Fat
Abnormal lipid level is common among women with PCOS and they possibly have higher risks of developing heart disease if it is not managed. Lower saturated fat intake can reduce cholesterol levels and improve heart health.
4. Regular physical activity
Regular exercise is effective at increasing energy output, managing metabolic markers including blood sugar, insulin, and lipid levels. Studies have found that combining physical exercise with lower calories diet is significantly associated with weight loss and reduction in blood sugar and insulin level.
To start exercising regularly, try the following:
- Walk to places that is within 1km,
- Park further, and walk to your destination,
- Schedule a 30-minute walk 1-2 times a day,
- Get more chances with staying active, including walking up and down stairs, housework, car washing, gardening, standing desk, walk and talk, walking your dog
- Set a goal, for example, 30 minutes cardio sessions 3 times a week
- Participate at strength or weightlifting training once a week, and increase as needed
Reference articles:
https://pubmed.ncbi.nlm.nih.gov/19062007/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8045367/
https://pubmed.ncbi.nlm.nih.gov/33849562/
https://academic.oup.com/jcem/article/98/12/4655/2834112
